SHOULDER REPLACEMENT SURGERY

The amount of shoulder replacement surgeries performed in the United States is increasing in number on a yearly basis, especially as our elderly population grows. It is estimated by the American Academy of Orthopaedic Surgeons that over 50,000 total shoulder replacements are performed in the U.S. yearly. The most common indication for performing a shoulder replacement is osteoarthritis of the glenohumeral (ball and socket) joint. This type of shoulder arthritis is usually due to a combination of age-related “wear and tear” occupations which require repetitive heavy lifting and overhead activity, previous trauma, genetics and gender (more common in females). Inflammatory arthritis conditions such as rheumatoid arthritis also lead to early deterioration of the shoulder joints.
Non-operative treatments for shoulder arthritis include anti-inflammatory and pain medications, physical therapy, activity modification and corticosteroid injections. When these methods are unable to significantly improve function and pain relief, a shoulder replacement surgery may be considered.
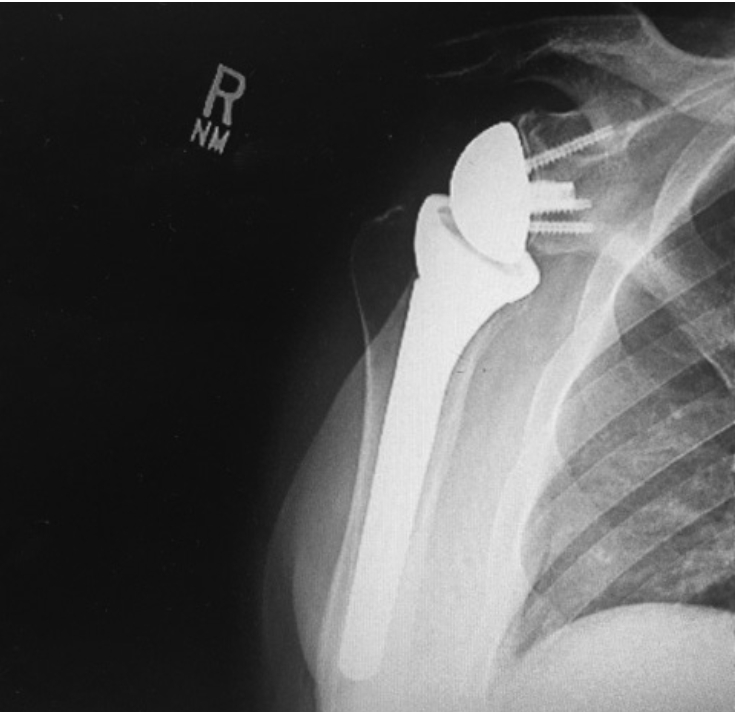
There are three main types of shoulder replacement surgeries commonly performed in the United States: a hemiarthroplasty, a standard total shoulder arthroplasty, and a reverse total shoulder arthroplasty.
1) A hemi-arthroplasty is a partial shoulder replacement in which only the humeral head (ball) is replaced with a metallic ball. This procedure is usually reserved for the treatment of fractures of the humeral head which cannot be fixed with a plate and screws, as well as for patients who are relatively young, where preserving bone for possible revision surgeries later in life may be an advantage.
2) A standard total shoulder replacement is a complete resurfacing of the ball and socket joint in which the shoulder socket is covered by a plastic liner which is impacted and usually cemented into place and a metallic ball with an attached rod is placed into the humerus after the bony ball is resected. This type of shoulder replacement requires that the rotator cuff tendons are intact and functional. The rotator cuff tendons are similar to bungee cords which keep the ball suspended and balanced in the center of the socket. These types of shoulder replacements have been reported to remain intact without the implants failing in 85-90 percent of patients for up to 15 years.
3) A reverse shoulder replacement is a procedure used primarily in patients who have shoulder joint arthritis and torn, irreparable rotator cuff tendons. In this procedure, the humeral head is resected and a metallic rod is inserted into the humerus with a cup attached to the top of it. The bony socket is replaced with a metallic ball with screws securing it, thereby “reversing” the ball and socket joint. The physics of aligning the replacement parts in this manner gives the replacement parts stability that would not be possible with a standard shoulder replacement. This type of replacement requires a functioning deltoid shoulder muscle as well as intact nerve function for the shoulder.
 As
previously mentioned, shoulder replacement surgeries are also performed
for fractures of the humeral head. These fractures account for
approximately 5 percent of all fractures and are the third most common
long-bone fracture type in the elderly. Whether or not to fix these
fractures with a plate and screws, treat them with a shoulder
replacement, or treat them conservatively without any surgery depends on
the amount the bone pieces are broken up and separated, the age and
activity level of the patient, and the overall health of the patient.
Shoulder replacements for treating fractures involve using either a
hemiarthroplasty or a reverse shoulder arthroplasty, depending on the
status of the rotator cuff tendons and the degree of bone destruction.
As
previously mentioned, shoulder replacement surgeries are also performed
for fractures of the humeral head. These fractures account for
approximately 5 percent of all fractures and are the third most common
long-bone fracture type in the elderly. Whether or not to fix these
fractures with a plate and screws, treat them with a shoulder
replacement, or treat them conservatively without any surgery depends on
the amount the bone pieces are broken up and separated, the age and
activity level of the patient, and the overall health of the patient.
Shoulder replacements for treating fractures involve using either a
hemiarthroplasty or a reverse shoulder arthroplasty, depending on the
status of the rotator cuff tendons and the degree of bone destruction.
An office evaluation for shoulder arthritis or a fracture consists of a physical exam to determine the range of motion, strength, integrity of the rotator cuff tendons, and nerve/vascular function of the upper limb. X-rays are performed to evaluate the degree of bone loss/joint space narrowing in arthritis and bony separation and destruction in fractures. A CT scan is sometimes needed to further evaluate the bony structures, especially in severe fractures, and an MRI is sometimes needed to define the condition of the rotator cuff tendons. If surgery is decided upon, pre-operative labs are performed to rule out any preexisting infection. A nerve block is often offered by the anesthesia physician just prior to the surgery to provide pain relief afterwards. Most patients only spend one night in the hospital after the surgery, and sometimes these procedures can be performed as “outpatient,” where the patient can go home the same day. Post-operatively, patients are usually instructed to use an arm sling for six weeks to protect certain tendon repairs performed during the replacement procedure. Physical therapy is initiated during the first week after surgery, with goals of restoring or improving strength, stamina and range of motion. It can take several months for a patient’s function to be maximized, and home exercises are often encouraged long-term to maintain that function. As function improves, pain typically subsides.
Like any other joint replacement procedure, shoulder replacement surgery can be successful in reducing/eliminating pain and improving function if performed for the proper reasons.
Dr. Carlton Houtz is an orthopaedic sports medicine surgeon at Highland Clinic Center of Orthopaedics and Sports Medicine who routinely performs shoulder replacement procedures. He can be reached at 798-4623, and his office is located at 1455 East Bert Kouns Industrial Loop, Suite 210, Shreveport. His office Web site is www.highlandclinic.com.
