Macular Degeneration: What is it, and how is it diagnosed?

Macular degeneration, or “age-related macular degeneration” (AMD), is one of the most common causes of vision loss n the United States and other industrialized countries. This disorder, which affects the center of the important film layer at the back of the eye, known as the macula, is a condition that often times has no symptoms early on. However, with time people may experience a worsening of the central vision, which makes daily activities of life such as reading and recognizing faces significantly harder. While AMD is a relatively common and sight-threatening condition, it can be a complicated and even scary topic for those not in the field of ophthalmology, including for patients and their loved ones.
So, what exactly is macular degeneration? As mentioned above, the macula is a critical structure in the eye that provides most of the central field of vision and plays an important role in color vision, contrast sensitivity and fine focus. AMD is a disease that typically occurs in older populations. It is believed that over a lifetime the components of the cells that make up the macula and its underlying support tissue (including the photoreceptor cells and retinal pigment epithelium tissue) undergo stress and damage which impacts their function in helping the center of vision work properly. Macular degeneration is conventionally broken up into two types – dry and wet.
The dry (or “non-exudative” or “nonneovascular”) type is the most common type and makes up about 90% of the disease in the population. Typically, on eye exam, one will find what are called “drusen,” or a cellular waste product underneath the macula. These “drusen” which appear as yellow-ish clumps are often times asymptomatic but can damage the macula over an extended time. In the most severe stage of “dry” AMD, known as “geographic atrophy,” patients will notice a decrease in vision, which can be profound. “Wet” AMD (or “exudative,” or “neovascular” AMD), while much less common than its “dry” counterpart, is responsible for a more rapid progression of advanced decline in vision. What happens in this form of the disease is that abnormal, “leaky” blood vessels start to grow up from underneath the macula and cause visual deterioration when they inevitably leak blood or fluid.
 While there is not a definite or exact cause of the disease, and research is still ongoing, it is accepted that age is the most important “risk” factor for macular degeneration. Patient population studies report that while approximately less than 2% of people under age 70 are diagnosed with AMD, the prevalence of the disease increases to as much as 12% in patients over 80 years old. Caucasian patients are more likely to be affected by AMD than patients of other races. Another important factor is family history, with the risk of AMD up to three times as high in those with a first-degree relative who is affected. Additional risk factors which are important, in that they can be modified and help reduce the risk of disease, are smoking and, to a lesser extent, poor diet.
While there is not a definite or exact cause of the disease, and research is still ongoing, it is accepted that age is the most important “risk” factor for macular degeneration. Patient population studies report that while approximately less than 2% of people under age 70 are diagnosed with AMD, the prevalence of the disease increases to as much as 12% in patients over 80 years old. Caucasian patients are more likely to be affected by AMD than patients of other races. Another important factor is family history, with the risk of AMD up to three times as high in those with a first-degree relative who is affected. Additional risk factors which are important, in that they can be modified and help reduce the risk of disease, are smoking and, to a lesser extent, poor diet.
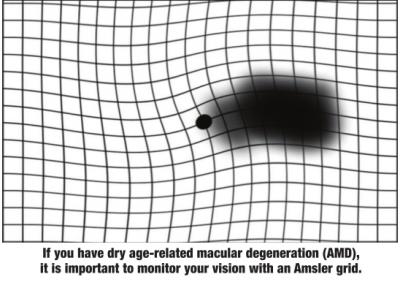
The diagnosis is generally made on a dilated eye exam with your eye-care provider. Patients, however, can help aid in the diagnosis or monitoring of disease by using an “Amsler grid,” which looks like a square grid or checkerboard, at home. Patients will look at this grid a couple of times a week, one eye at a time, and look to see if the lines appear straight. If they appear wavy, or there is a blank spot in the visual field, please notify your provider, as this can be a sign of worsening AMD.
Unfortunately, there is no definite cure at this time for visual loss that has already occurred. In patients with the earlier stages of “dry” AMD, antioxidant vitamins and minerals can be helpful in slowing progression of the disease. In patients with “wet” AMD, there are medications known as “anti-VEGF medications,” which are injected directly into the eye, which can help stop the formation of the previously mentioned leaky blood vessels and slow the worsening of vision. At the end of the day, the overall health benefits of eating healthy, exercise and quitting smoking cannot be understated.
Age-related macular degeneration can notably impact the quality of life of its patients and their loved ones. For that reason, it is important to spread awareness and education of this condition, especially as people are living longer and the number of those affected is expected to rise.
Bilal Shaukat, MD, is a third-year ophthalmology resident at LSU Health Shreveport.
References:
“Age-Related Macular Degeneration PPP – Updated 2015.” American Academy of Ophthalmology. 2015-01-29. Retrieved 2018-11-13.
“Facts About Age-Related Macular Degeneration.” National Eye Institute. June 2015. Archived from the original on 22 December 2015. Retrieved 21 December 2015.
Mehta S (September 2015). “Age-Related Macular Degeneration.”
Primary Care. 42(3): 377–91. doi:10.1016/j.pop.2015.05.009 Kanski, J. J., Bowling, B., Nischal, K. K., & Pearson, A. “Acquired Macular Disorders.” Clinical Ophthalmology: A systematic approach (8th ed.). Edinburgh; New York: Elsevier/Saunders. 2016. 598-603. Print.
