Proton Therapy

For prostate cancer
Willis-Knighton Cancer Center’s Department of Radiation Oncology became the first site in the world to introduce compact scanning beam imageguided proton therapy. Over subsequent years, renowned centers such as Mayo Clinic, St. Jude’s, Memorial Sloan Kettering Cancer Center and Johns Hopkins Medical Center followed suit. The Proteus ® ONE at Willis-Knighton remains the only proton therapy machine in Louisiana.
One of the most common indications for proton therapy is prostate cancer. Prostate cancer is the second leading cause of cancer death among men in the United States, but it has an outstanding survival rate when detected early. Prostate cancer develops in the prostate gland, which is located beneath the bladder and in front of the rectum and can cause both local symptoms and spread to other parts of the body. For early-stage prostate cancer, radiation therapy, delivered with a number of techniques, and surgery (known as the radical prostatectomy), have similar outcomes and are favorable treatment options. For more locally advanced prostate cancer, radiation therapy is a preferable approach and is often combined with hormonal therapy.
The overall benefits of proton therapy are: 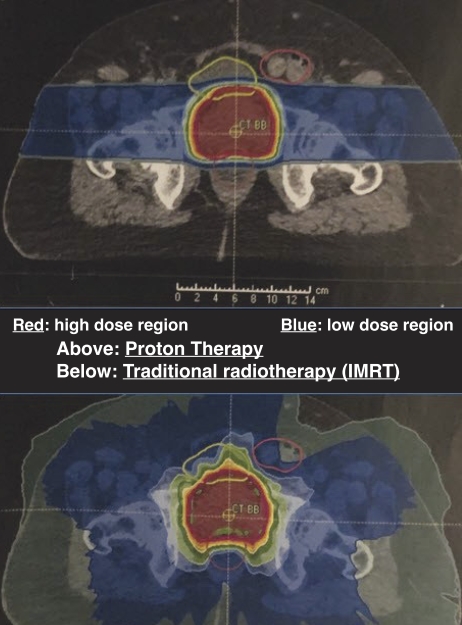
• Precise and accurate delivery of high radiation dose to kill cancer cells in the prostate and surrounding tissues.
• Minimal impact to healthy tissues and vital organs surrounding the prostate.
• Non-invasive treatment without surgery with patients often working throughout the course.
• A proven technique used for prostate cancer since the early 1990s.
The National Comprehensive Cancer Network (NCCN) practice guidelines describe proton therapy as an effective form of external beam radiation therapy. Many studies have demonstrated that traditional radiation therapy and proton therapy are equally effective in eliminating prostate cancer, with proton therapy significantly reducing dose exposure to the surrounding healthy tissues.
Most men who are candidates for intensity-modulated radiation therapy (IMRT) or brachytherapy (seed implants) are also candidates for proton therapy. Side effects associated with proton therapy can be localized skin changes, fatigue, changes in bowel or bladder function that are typically transient, or erectile dysfunction. Treatment can be delivered over four to nine weeks depending upon the patient and their individual circumstances. Numerous quality of life (QOL) studies comparing radiation therapy to surgery have demonstrated that radiation therapy has improved patient satisfaction in both potency (the ability to maintain an erection) and incontinence (leakage). In particular, proton therapy can reduce the radiation dose to normal tissues surrounding the prostate to a degree previously impossible with 3D conformal or IMRT techniques. As less healthy tissue is exposed to radiation, there is also a reduction in the risk of treatment-related second malignancies, which is particularly relevant for younger men who elect to undergo radiotherapy and avoid surgery.
The reason proton therapy is advantageous over traditional approaches is due to a physics property known as the Bragg peak. The Bragg peak is a phenomenon whereby protons unload all cancer-killing energy at a certain depth in the body. Because protons are heavy particles, they only deliver a low dose of radiation therapy as they pass through the body, ultimately depositing all of their energy into a cancer before the particle is annihilated. As the proton has been destroyed, there is no exit dose to surrounding tissues. This concept can best be explained by imagining a fuel truck crashing into a snowbank. The truck is so heavy that it easily displaces the snow but eventually, it will slow until coming to a stop where the truck explodes.
Because the proton beam can be very precisely controlled using high-energy magnets and advanced computers, doctors can often prescribe a higher dose of radiotherapy to the target with a lesser impact on healthy structures. This is in contrast to X-rays delivered by conventional radiotherapy. An X-ray passes completely through the body, explaining why your bones are projected onto a film behind a patient with X-rays but not with protons.
Many cancer centers, including Willis-Knighton Cancer Center, routinely use other devices such as implanted fiducial markers and specialized gels to further protect the critical surrounding organs and improve the precision of therapy.
Proton therapy has been compared with photon (X-ray) therapy in numerous body sites with a large series reporting reduced acute adverse events, less unplanned hospitalizations with similar disease-free and overall survival (JAMA Oncology 2020, Brian Baumann et al). Proton therapy has also demonstrated excellent prostate cancer control rates. One study (Genitourinary Cancer May 2016 Nancy Mendenhall et al) reviewed almost 1,400 patients and found that the fiveyear freedom from cancer progression was 99% and 94% in low-risk and intermediate-risk treated prostate cancer patients. For patients with more advanced prostate cancer where the pelvic lymph nodes need to be treated, proton therapy has a dramatic dose exposure benefit with a greatly reduced risk of bowel damage.
The Proteus ® ONE proton unit at Willis-Knighton is managed by a dedicated team of experienced medical physicists and specially trained dosimetrists and therapists. Five board-certified radiation oncologists oversee therapy and are available for both rapid consultations and second opinions working in conjunction with Willis-Knighton urologists. Willis- Knighton Cancer Center also serves as an international training site for proton therapy centers and has welcomed hundreds of physicians and physicists.
Lane R. Rosen, MD, FACRO, is the director of the Department of Radiation Oncology at Willis-Knighton Health System.
The national COMPPARE Trial is available at Willis-Knighton Cancer Center and is evaluating the efficacy of proton therapy to determine if prostate cancer patients treated with proton therapy as compared to more traditional options experience improved quality of life, reduced toxicity or non-inferior or even superior cancer control. For more information or to see if you qualify, contact the Willis-Knighton Cancer Center Research Department at (318) 212-8671.
