A Medical Pioneer

Dr. George Merriman and laparoscopic surgery
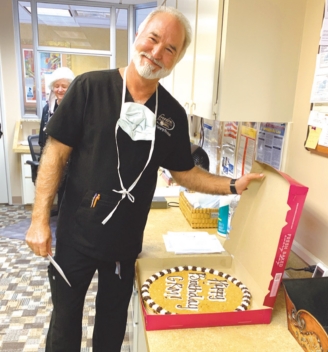
Dr. George Merriman II has been looking into people’s lives for all his 30 years as a physician … literally. He is marking 30 years as an M.D. and has played a significant role in pioneering new surgical methodology in our area.
“I’m a general surgeon. My focus for the last 25 years has been bariatric surgery,” he said. Bariatric surgeries, like gastric bypass and other weight loss surgeries, are indicated when a patient cannot lose excess weight through diet and exercise.
 Merriman’s work has been as a pioneer in the field of laparoscopic surgery, which came into common practice just as he was finishing his medical training. Laparoscopy examines the organs of the abdomen or other enclosed spaces in the body. Typically, it’s described as a low-risk, minimally invasive procedure that requires only small incisions, thus reducing recovery time.
Merriman’s work has been as a pioneer in the field of laparoscopic surgery, which came into common practice just as he was finishing his medical training. Laparoscopy examines the organs of the abdomen or other enclosed spaces in the body. Typically, it’s described as a low-risk, minimally invasive procedure that requires only small incisions, thus reducing recovery time.
Merriman finished his training at the University of Alabama/Birmingham, a leader in training physicians and surgeons, in 1992. At the time, the pioneers of laparoscopy in Shreveport were L. Keith Mason Jr. and Charles Itzig.
“They had performed the first laparoscopic cholecystectomy [gall bladder surgery],” Merriman explained. “And they were [also doing] laparoscopic hernia repairs. I joined them and did one of the first laparoscopic reflux surgeries. It was called a Nissen fundoplication.” By the late 1990s, Merriman pioneered laparoscopic bariatric surgery in this region.
In the early 2000s, robotic surgery blossomed, initially used by urologists to treat prostate disorders. “It was very rapidly popular,” according to Merriman, “because you can do better, you can see better, you have several additional degrees of freedom. I was the first surgeon in this region to train on what’s now called the DaVinci Robot.”
Rather than being the plot of a Dan Brown novel, a DaVinci Robot gets its name because the famous artist is known for his study of human anatomy, which led to the design of the first robot.
 Merriman explained the utility of the robot in surgery. “Bariatric surgery is challenging in the hierarchy of surgeries.
Merriman explained the utility of the robot in surgery. “Bariatric surgery is challenging in the hierarchy of surgeries.
It’s not like taking an appendix out or taking a gall bladder out.”
He said the current version of the robot has what he calls many degrees of freedom which are of great benefit to patient and surgeon alike.
Traditionally, bariatric surgery required a large incision in the patient’s abdomen. The physician then had to literally look around inside the patient to diagnose, evaluate and repair what was happening inside the tight environment of a person’s body. “Like a gastric bypass surgery, you’re working in two distinct areas in the abdominal cavity,” Merriman explained, and the robot makes those surgical contortions much easier. “I can initially be looking in the upper part of the abdomen, and then without having to do anything with other than my hands, I can look down into the lower abdomen. When I say degrees of freedom, that’s what I mean.” And that freedom is easier on the surgeon and makes recovery time shorter due to the lack of large, invasive abdominal incisions.
Merriman said the major advantage of robotic surgery is in teaching, whether it’s surgery residents or training other surgeons. “To teach before, you had to let that only partially trained individual just go at it, and you’d have to watch them. With the robot, it’s just so much simpler to say, ‘No, move your hand this way,’ to let them go and work through the learning curve knowing that at any moment I can push a button and intervene, and I’m in control of everything. The safety factor of teaching is just increased exponentially.”
And that’s not the only benefit. “The thing for an old,
grizzled surgeon is the load, the stress and strain it takes off your
body, especially for laparoscopic surgery. You’re always twisting and
torquing. It’s a real load on the low back and especially the hands and
the arms and the shoulders. That just disappears with a robot. So, that
will extend careers because of the lack of physical limitations and
maladies.”
After 30 years, it’s natural to think about retirement. Merriman went to high school in Shreveport at Jesuit High School. His wife is from Dallas, so her family is also close. The allure of Shreveport is what kept them. “I didn’t want to be in a big city. So many of my old friends are still in town. It’s such a great place to raise kids. This is a 15-minute city. You can get pretty much get anywhere in 15 minutes. The lifestyle is what has kept me here.”
Why so long in this demanding career? Merriman explains it this way: “The thing with surgery, I think, unlike other areas of
medicine, maybe, it’s like being a professional athlete. It’s the juice.
You’re going in. Every case is a potential real challenge. And even
though you’ve done it a thousand times before, there’s just a pleasure, a
satisfaction, a gratification; it’s hard to let go of. There’s no
‘gimme,’ and you’ve got to go in with your game on. It doesn’t matter if
you’re tired. And somehow, the juice always shows up. I get in there,
and suddenly, I’m not fatigued, I’m not tired. I’m focused, I’m good to
go.”
Besides, George Merriman is looking to do more than hang up his robot and go fishing. “All the things I’ve done, all I’ve created, I took the work that [Mason and Itzig] had done and pushed it to the next level. Then I took the work that [Dr.] Kenneth Jones was doing with the bariatrics. I’m looking for how to build a continuation, my legacy, of what I’ve been able to accomplish here. That’ll be a way to stay in the game and not have to be a front-line guy.”
